Can Your Gut Predict Depression?
Depression symptoms affect more than 280 million people worldwide, according to the World Health Organization. While often framed as purely mental or emotional, scientists are uncovering groundbreaking evidence that the origins of depression may also lie in the gut. This new understanding centers on the gut-brain axis, a complex communication system between the digestive tract and the brain. Could your gut microbiome predict depression before it manifests? Recent studies suggest the answer might be yes.
This article explores the latest science on depression symptoms, gut health and depression, microbiome and mood, psychobiotics, bipolar disease, signs of depression, antidepressants, and clinical depression. We’ll dive deep into each topic, connecting the dots between diet, lifestyle, mental health, and the fascinating world of the gut microbiome.
Depression Symptoms and the Gut-Brain Axis
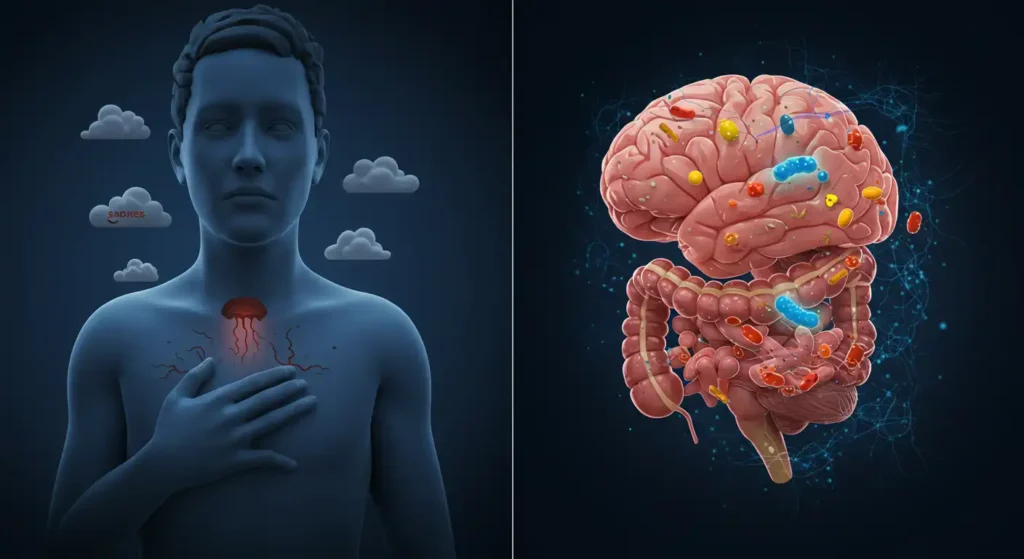
When we talk about depression symptoms, the first things that come to mind are emotional: persistent sadness, loss of interest, or hopelessness. However, modern neuroscience and gastroenterology reveal that these symptoms are not confined to the brain. The gut-brain axis a two-way communication system between the gut microbiome and the central nervous system is redefining how we understand depression.
The Biological Foundation of the Gut-Brain Axis
The gut-brain axis involves neural, hormonal, and immune pathways. The vagus nerve acts as the main highway, transmitting messages between gut and brain. Interestingly, the gut produces about 90% of the body’s serotonin, a neurotransmitter critical for mood regulation. If gut bacteria become imbalanced (a condition called dysbiosis), they reduce serotonin production, influencing clinical depression.
📖 A landmark study in Nature Microbiology found that people with major depressive disorder had fewer strains of beneficial bacteria, particularly those producing anti-inflammatory metabolites (Nature Microbiology).
Depression Symptoms with a Gut Link
Beyond emotional struggles, depression often shows physical symptoms linked to digestion:
- Bloating, constipation, or diarrhea.
- IBS-like discomfort.
- Reduced appetite or emotional eating.
- Fatigue linked to poor nutrient absorption.
The overlap between depression symptoms and gut dysfunction suggests the microbiome plays a predictive role.
The Role of Inflammation
Gut bacteria release metabolites that can trigger or reduce inflammation. Harmful bacteria increase cytokines pro-inflammatory molecules that travel through the bloodstream and cross the blood-brain barrier. Researchers now see chronic inflammation as one of the key mechanisms behind clinical depression..
📖 Research published in Psychiatry Research confirms that inflammatory markers are elevated in many patients with depression (Psychiatry Research).
The Vagus Nerve and Depression
The vagus nerve, stretching from brainstem to gut, regulates mood through electrical signaling. Clinical use of vagus nerve stimulation (VNS) already exists for treatment-resistant depression, confirming the gut-brain axis is more than theoretical.
Practical Implications
This understanding shifts treatment from brain-centered to body-wide approaches:
- Probiotic therapy to restore microbiome balance.
- Anti-inflammatory diets.
- Stress reduction methods like yoga and meditation that also affect gut function.
Gut Health and Depression Symptoms – The Role of Diet and Lifestyle

The saying “you are what you eat” gains new weight when discussing gut health and depression. Nutrition directly affects the microbiome, which in turn influences depression symptoms.
How Diet Shapes Mental Health
- Western Diet: High in processed foods, sugar, and trans fats → promotes inflammation.
- Mediterranean Diet: Rich in vegetables, legumes, fish, and olive oil → lowers depression risk.
- Fiber and Prebiotics: Feed beneficial gut bacteria, improving mood.
- Fermented Foods: Yogurt, kefir, kimchi, and sauerkraut introduce probiotics that enhance microbiome diversity.
📖 The SMILES Trial (BMC Medicine) demonstrated that participants with clinical depression who switched to a Mediterranean diet experienced significant mood improvements (BMC Medicine).
Nutrients Essential for Reducing Depression Symptoms
- Omega-3 fatty acids: Reduce inflammation, improve brain plasticity.
- Magnesium and Zinc: Linked to neurotransmitter balance.
- Vitamin D: Deficiency strongly associated with depression.
- Polyphenols: Found in berries, tea, and dark chocolate, they act as antioxidants protecting brain and gut.
Lifestyle Factors Beyond Diet
- Exercise: Boosts microbiome diversity and serotonin.
- Sleep: Poor sleep disrupts gut flora and worsens depression symptoms.
- Stress: Increases cortisol, damaging gut lining and altering microbiota.
Depression Symptoms, Microbiome and Mood – The Rise of Psychobiotics
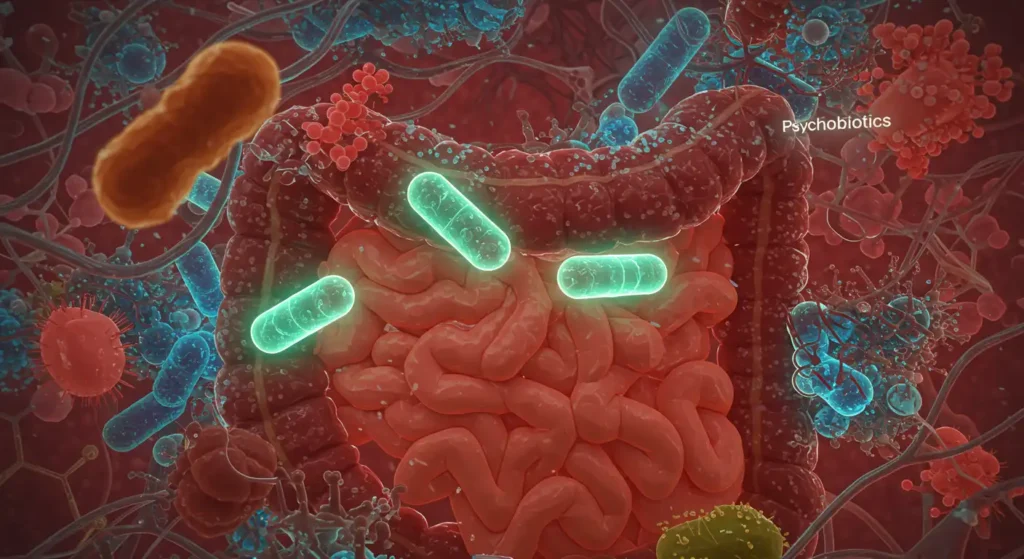
For decades, scientists viewed the brain and gut as two independent systems. Today, however, research has revealed that the two are deeply intertwined through what is known as the gut-brain axis. This connection means that the trillions of bacteria, fungi, and microorganisms residing in the gut microbiome don’t just regulate digestion they can directly influence our mood, stress levels, and even mental health conditions such as anxiety and depression. A growing body of evidence has led to the rise of a new concept in nutritional psychiatry: psychobiotics.
Psychobiotics are a class of probiotics and prebiotics specifically designed to influence mental well-being by restoring balance in the gut microbiome. Unlike traditional probiotics that primarily support digestion, psychobiotics target the gut-brain axis, helping regulate neurotransmitters like serotonin, dopamine, and GABA chemicals that are essential for mood stabilization and emotional health.
The Gut-Brain Connection: How Microbes Talk to the Mind
The gut and brain communicate through multiple channels:
- The Vagus Nerve – This cranial nerve acts as a communication superhighway, sending real-time messages between the gut and the central nervous system.
- Neurotransmitters – The gut produces up to 90% of the body’s serotonin, the “happiness hormone. Similarly, bacteria in the gut can influence GABA, a neurotransmitter that calms the nervous system.
- Immune System Pathways – An imbalanced microbiome can trigger inflammation, which researchers link to depression and anxiety.
- Metabolites and Short-Chain Fatty Acids (SCFAs) – Healthy gut bacteria produce SCFAs that protect the blood-brain barrier and influence brain chemistry.
This two-way communication means that a disrupted microbiome can lead to mood disorders, while a balanced gut ecosystem can promote resilience against stress.
The Science Behind Psychobiotics
Psychobiotics are not science fiction they are backed by clinical trials and growing medical research. For example, certain strains of Lactobacillus rhamnosus actively reduce anxiety-like behavior in both animals and humans. Another strain, Bifidobacterium longum 1714, has been associated with improved stress resilience and reduced cortisol levels.
In a groundbreaking study published in Frontiers in Psychiatry (2019), researchers found that psychobiotics improved not only gut health but also cognitive performance, emotional regulation, and sleep quality. These results suggest that psychobiotics could be a natural alternative or at least a strong complement—to antidepressants and anti-anxiety medications.
Benefits of Psychobiotics for Mental Health
The rise of psychobiotics is linked to their wide range of benefits for mood and brain function:
- Reduction of Stress and Anxiety – Psychobiotics lower cortisol (the stress hormone) and improve the body’s ability to adapt to daily pressures.
- Improved Sleep Quality – By regulating melatonin and serotonin, psychobiotics promote deeper, more restorative sleep.
- Enhanced Cognitive Function – Research suggests psychobiotics improve focus, memory, and decision-making by reducing neuroinflammation.
- Mood Stabilization – Balanced gut flora helps regulate neurotransmitter levels, which reduces the risk of depression and mood swings.
- Support During Depression – Early studies show that psychobiotics may complement therapies for clinical depression, offering a natural route for symptom relief.
Natural Sources of Psychobiotics
Psychobiotics can be obtained through supplementation or food sources. Some of the most effective psychobiotic-rich foods include:
- Fermented Foods – Yogurt, kefir, kimchi, sauerkraut, miso, and tempeh provide strains of beneficial bacteria.
- High-Fiber Foods (Prebiotics) – Oats, bananas, garlic, onions, and asparagus feed healthy gut bacteria, helping psychobiotics thrive.
- Specialized Probiotic Supplements – Formulas specifically labeled as psychobiotics often include strains such as Lactobacillus helveticus R0052 and Bifidobacterium longum 1714.
Incorporating these foods daily can help foster a balanced microbiome that supports both gut and brain health.
The Future of Psychobiotics
The field of psychobiotics is still relatively new, but its potential is enormous. Future research is expected to expand in areas such as:
- Personalized Psychobiotics – Supplements tailored to an individual’s microbiome composition.
- Adjunct Therapies – Psychobiotics working alongside conventional psychiatric treatments.
- Prevention of Mental Illness – Early interventions with psychobiotics to reduce the risk of depression, anxiety, and even neurodegenerative diseases.
Psychobiotics represent a paradigm shift in mental health treatment, emphasizing natural and preventive care rather than focusing solely on symptom suppression.
Lifestyle Factors That Support Psychobiotic Benefits
To maximize the effect of psychobiotics, it’s crucial to adopt habits that support gut health:
- Balanced Diet – Minimize processed foods and sugar while prioritizing whole, plant-based meals.
- Regular Exercise – Physical activity stimulates microbial diversity and lowers stress hormones.
- Stress Management – Mindfulness, meditation, and yoga reduce gut inflammation triggered by chronic stress.
- Quality Sleep – Poor sleep disrupts the gut microbiome, weakening the impact of psychobiotics.
- Reduced Antibiotic Overuse – While necessary in certain cases, antibiotics can wipe out beneficial bacteria, reducing psychobiotic effectiveness.
Depression Symptoms, Bipolar Disease, and Clinical Depression – The Gut Connection
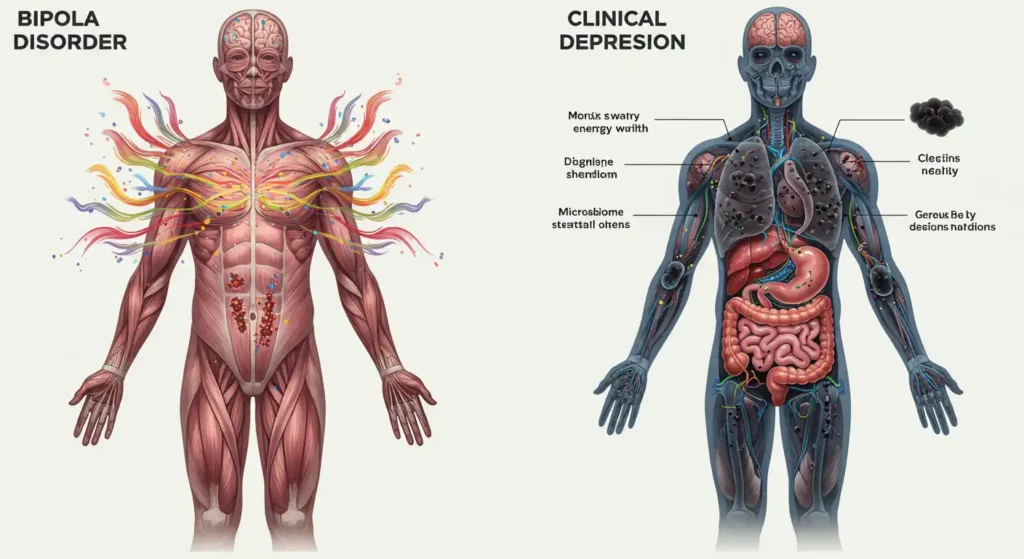
In recent years, a groundbreaking area of research has emerged in neuroscience and psychiatry: the profound connection between gut health and mental health. Scientists are increasingly referring to the gut as the “second brain”, given its complex network of neurons, neurotransmitter production, and constant communication with the central nervous system through the gut-brain axis. This relationship is now being explored as a key factor in mood disorders, particularly depression, bipolar disorder, and clinical depression.
Understanding the Gut-Brain Axis in Mood Disorders
The gut-brain axis is a bidirectional communication system between the enteric nervous system (ENS) in the gut and the central nervous system (CNS). This intricate network involves the vagus nerve, immune system, endocrine signaling, and microbiome metabolites. What makes this connection so fascinating is the realization that gut microbes not only assist digestion but also produce neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), all of which play crucial roles in regulating mood.
Studies have shown that over 90% of serotonin a neurotransmitter often referred to as the “happiness chemical”—is produced in the gastrointestinal tract. When the gut microbiome becomes imbalanced (a condition known as dysbiosis), serotonin regulation may be disrupted, increasing vulnerability to depression and bipolar mood swings.
Depression Symptoms and the Gut Connection
Depression is one of the most studied conditions in relation to the gut microbiome. Patients with depression often show altered gut microbial composition, including a decrease in beneficial bacteria such as Bifidobacterium and Lactobacillus. These bacteria are known for producing short-chain fatty acids (SCFAs) like butyrate, which not only support gut barrier integrity but also reduce inflammation in the brain.
Chronic inflammation, sometimes triggered by a “leaky gut,” is considered a major factor in the pathogenesis of depression. Research suggests that intestinal permeability allows pro-inflammatory molecules to enter circulation, affecting brain function and leading to depressive symptoms. This phenomenon is sometimes referred to as the “inflammatory hypothesis of depression.”
Additionally, certain probiotics often called psychobiotics have demonstrated positive results in clinical trials. Supplementation with specific strains, like Lactobacillus helveticus and Bifidobacterium longum, has been shown to reduce depressive symptoms, improve stress resilience, and regulate cortisol levels.
Bipolar Disorder and Gut Health
Bipolar disorder, characterized by alternating episodes of depression and mania, has also been linked to gut microbiome imbalances. Recent studies indicate that individuals with bipolar disorder tend to exhibit reduced microbial diversity and increased levels of pro-inflammatory bacteria.
This imbalance can influence dopaminergic signaling in the brain a critical pathway in regulating mood swings. Emerging evidence suggests that patients with bipolar disorder have higher rates of gastrointestinal issues, such as irritable bowel syndrome (IBS), compared to the general population, pointing to a strong gut connection.
Moreover, treatments commonly prescribed for bipolar disorder, including mood stabilizers and antipsychotics, may themselves alter gut microbiota composition, creating a complex feedback loop. Researchers are now investigating whether microbiome-targeted therapies could complement conventional psychiatric medications, potentially reducing side effects and improving long-term outcomes.
Clinical Depression and Long-Term Gut-Brain Dysregulation
When depression becomes chronic and treatment-resistant, it is often classified as clinical depression or major depressive disorder (MDD). This severe condition does not always respond well to traditional antidepressants, which primarily target neurotransmitters in the brain.
Here, the gut-brain axis offers new hope. Research suggests that individuals with MDD frequently exhibit gut dysbiosis, systemic inflammation, and altered production of microbial metabolites. These imbalances can impair the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s stress response. Over time, chronic HPA axis activation worsens depressive symptoms and may lead to cognitive decline.
New therapeutic strategies include:
- Fecal microbiota transplantation (FMT), where gut bacteria from healthy donors are introduced into the patient’s gut. Preliminary trials show promising mood improvements.
- Dietary interventions, such as the Mediterranean diet, which is rich in fiber, omega-3 fatty acids, and antioxidants that nourish beneficial microbes.
- Precision psychobiotics, tailoring probiotic and prebiotic supplementation to specific gut profiles.
This personalized medicine approach could mark a turning point in how we treat chronic and treatment-resistant depression.
Practical Strategies for Supporting Gut Health and Mental Well-Being
While research continues to expand, individuals struggling with depression, bipolar disorder, or clinical depression can adopt strategies to support gut and mental health simultaneously:
- Increase fiber intake → Foods rich in prebiotics, such as oats, onions, garlic, and bananas, feed beneficial bacteria.
- Consume fermented foods → Yogurt, kefir, sauerkraut, and kimchi naturally introduce probiotics into the gut.
- Limit processed foods and sugar → These encourage growth of harmful bacteria linked to inflammation and mood instability.
- Consider probiotic supplements → Specific strains such as Bifidobacterium longum and Lactobacillus rhamnosus are well-studied in mental health.
- Manage stress and sleep → Poor sleep quality and chronic stress disrupt the gut-brain axis. Practices like meditation and yoga improve both.
- Seek professional guidance → Collaboration between psychiatrists, nutritionists, and gastroenterologists ensures a holistic treatment plan.
Depression Symptoms, Antidepressants, and the Future of Gut-Based Therapy
Depression is one of the most common mental health conditions worldwide, affecting more than 280 million people globally according to the World Health Organization (WHO, 2023). Traditionally, researchers have long viewed depression as a purely psychological or neurological disorder, often linking it to neurotransmitter imbalances like low serotonin, norepinephrine, or dopamine. However, emerging research in gut-brain axis science is transforming how we understand depression. Studies suggest that gut health, specifically the balance of the gut microbiome, plays a crucial role in regulating mood, cognition, and even response to antidepressant treatment.
This new perspective is fueling interest in gut-based therapies, including probiotics, prebiotics, dietary changes, and even fecal microbiota transplantation (FMT) as potential complementary or alternative treatments for depression. But before diving into future therapies, it’s important to clearly recognize the expanded signs of depression, understand the current role of antidepressants and combined therapies, and explore the promising horizon of personalized psychiatry through microbiome testing.
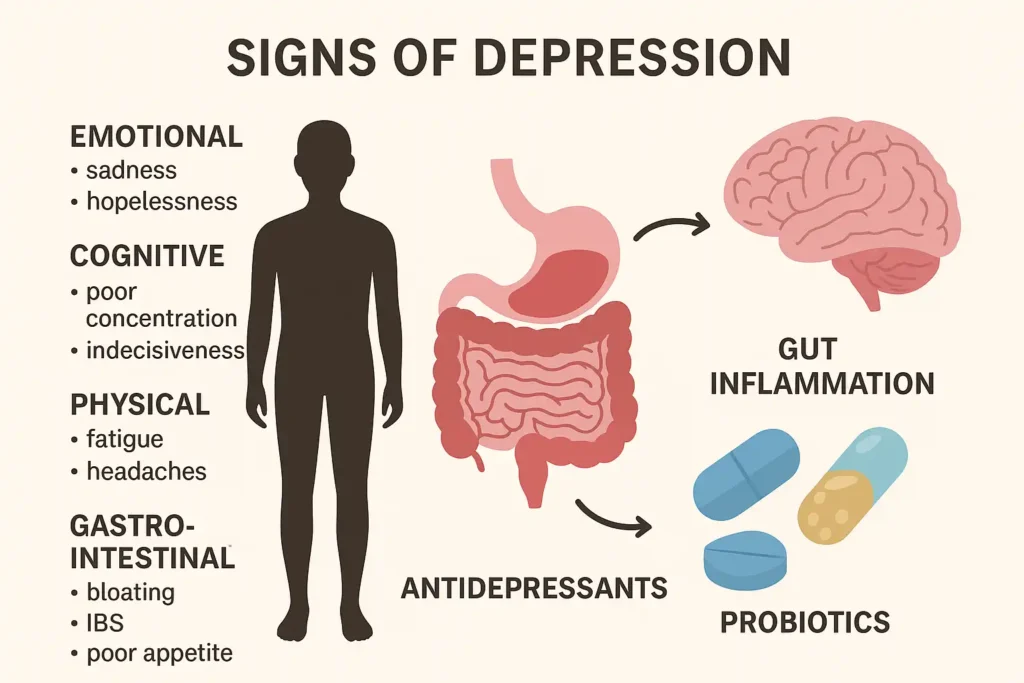
Expanded Depression Symptoms
Depression is not a one-size-fits-all condition. It manifests differently across individuals and cultures, and symptoms can range from emotional struggles to cognitive dysfunction, physical health problems, and even gastrointestinal disturbances linked to gut imbalance. For SEO purposes, let’s break down the signs of depression into key categories.
1. Emotional Depression Symptoms
- Persistent sadness: A deep feeling of emptiness or hopelessness lasting weeks or months.
- Loss of interest (anhedonia): Reduced pleasure in activities once enjoyed, such as hobbies, food, or socializing.
- Feelings of worthlessness or guilt: Intense self-criticism, sometimes linked to childhood experiences or trauma.
- Hopelessness about the future: A belief that nothing will improve, which increases suicide risk.
Emotional depression symptoms are often the most visible but not the only indicators.
2. Cognitive Symptoms of Depression
- Poor concentration: Difficulty focusing on tasks, reading, or holding conversations.
- Indecisiveness: Struggling to make even small choices, such as what to eat.
- Memory issues: Forgetfulness and reduced short-term memory linked to impaired hippocampal function.
- Rumination: Repetitive negative thinking that reinforces depressive states.
Cognitive dysfunction is often underestimated but plays a large role in workplace productivity loss and academic struggles among those with depression.
3. Physical Symptoms of Depression
- Chronic fatigue: Constant tiredness even after rest, due to disrupted sleep and inflammation.
- Headaches and migraines: Stress-related headaches are common among those with depression.
- Muscle pain and tension: Depression often manifests with somatic pain symptoms.
- Changes in appetite: Overeating (comfort eating) or undereating, leading to weight fluctuations.
These physical symptoms show that depression is not just in the mind but affects the whole body, often linked to inflammation markers such as cytokines.
4. Gastrointestinal Depression Symptoms
- Bloating: Poor gut motility linked to stress hormones.
- Irritable Bowel Syndrome (IBS): Up to 60% of IBS patients also meet criteria for anxiety or depression.
- Poor appetite and nausea: Loss of desire to eat, sometimes triggered by microbiome imbalance.
- Diarrhea or constipation: Dysregulated gut microbiota can influence bowel movements and worsen mood.
Antidepressants and Combined Therapies
While gut-based therapies are on the rise, antidepressants remain the gold standard in clinical practice. Medications such as SSRIs (Selective Serotonin Reuptake Inhibitors), SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors), and tricyclic antidepressants are prescribed globally to millions of patients. However, effectiveness varies about 30-40% of patients with depression do not respond fully to antidepressants (National Institute of Mental Health, 2022).
This has led researchers to explore combined therapies:
- Antidepressants + Probiotics: Probiotics may improve the efficacy of SSRIs by restoring gut microbiota balance. Clinical trials show that certain strains like Lactobacillus helveticus and Bifidobacterium longum can reduce depressive symptoms when combined with antidepressants.
- Dietary Interventions: The Mediterranean diet, rich in fiber, omega-3 fatty acids, and polyphenols, has been linked to lower depression rates and better antidepressant outcomes.
- Psychotherapy + Gut Care: Cognitive Behavioral Therapy (CBT) alongside gut microbiome support may improve long-term outcomes compared to therapy alone.
- Exercise + Microbiome Boost: Physical activity enhances both brain function and microbial diversity, creating a dual benefit for depression management.
The takeaway? Future depression treatments will likely combine medications with gut-health interventions, creating a holistic approach to healing.
The Future of Personalized Psychiatry
One of the most exciting frontiers in depression treatment is personalized psychiatry, powered by gut microbiome testing. Instead of the current trial-and-error method of prescribing antidepressants, doctors may soon use biomarkers from gut bacteria to predict which therapies will be most effective.
Key innovations in this field include:
- Microbiome Testing for Depression Risk
- Stool sample analysis can identify microbial imbalances linked to higher depression risk.
- Companies are developing gut health kits that could eventually integrate into psychiatric diagnostics.
- Tailored Probiotics as Prescriptions
- Instead of general probiotics, psychiatrists could prescribe specific strains linked to serotonin production or stress reduction.
- For example, Bifidobacterium breve has been studied for its anxiolytic effects, while Lactobacillus rhamnosus may regulate GABA, the brain’s calming neurotransmitter.
- Preventive Psychiatry via Gut Health
- Public health strategies may focus on gut-friendly diets, early probiotic interventions in children, and reducing antibiotic overuse.
- This could lower global depression rates by targeting root causes rather than just symptoms.
- AI and Gut Data
- Artificial intelligence could help analyze microbiome data, creating customized gut-brain health programs for individuals.
- This precision medicine approach may revolutionize psychiatry in the next decade.
Conclusion – Your Gut May Hold the Key to Mental Health
The science is clear: the microbiome influences mood, stress, and depression symptoms. By improving gut health through diet, lifestyle, and psychobiotics, we may not only treat but also prevent clinical depression and related mood disorders.






